TECHNOLOGY
Smarter platforms transforming benefits administration
Image
Complex challenges, clear answers
Consultative Approach
Aptia takes the time to understand your specific benefits program needs and tailors our dependent eligibility verification audits to ensure maximum accuracy and savings.
Image
Customization to Meet Your Needs
We offer flexible audit solutions that integrate seamlessly with your existing benefits program, adapting to your unique requirements.
Video file
Expert Service
Our experienced team delivers high-touch, responsive service, guiding you through every step of the audit process and ensuring the highest level of satisfaction and success.
Image
Our use of AI
Modern technology advances benefits administration by improving efficiency and enabling early detection of risks across complex systems.
Image
Employee interactions
Participants can engage 24/7 to complete enrollment or life event tasks from any device, on their own schedule, with guidance available every step of the way.
Image
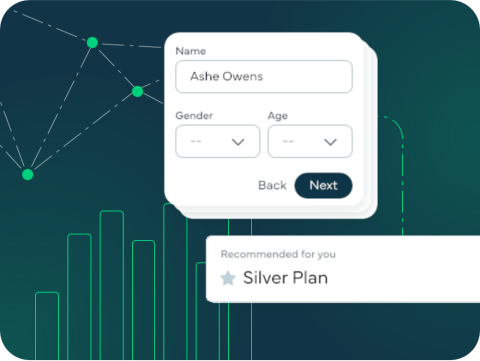
Decision support
Our predictive tools match employees with plans that align to their needs and budget. This helps them become better benefits consumers and results in improved health and cost outcomes.
Image
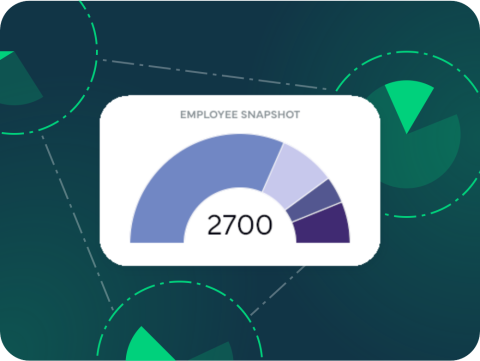
Data accuracy
Our platform promotes data accuracy through seamless system integration, ensuring timely coverage, fewer errors, and visibility into key benefit, carrier, and population trends, helping HR stay ahead.
Image
Security, Quality, & Data Management
Protect your data so you can use it to supercharge your business.
Image

Compliance
See how we can help make it easy to adhere to complex regulations, without the headache.
FAQ
What is dependent eligibility verification?
Dependent eligibility verification (DEV) is the process of auditing the dependents listed on your healthcare plans to confirm they are eligible for coverage under your benefits program.
What are the benefits of conducting a dependent eligibility verification audit?
DEV audits help organizations save costs, maintain compliance, and ensure that only eligible dependents are receiving benefits, preventing fraud and unnecessary expenses.
How often should I conduct a dependent eligibility verification audit?
It’s recommended to perform a DEV audit annually or whenever there are significant changes to your benefits plan. Ongoing maintenance, such as verifying new hires, life events, and conducting re-verification projects every 3-4 years, ensures continued accuracy and cost savings.
How will this solution improve my company’s benefits strategy?
With our solution, companies can align their benefits strategy with delivery and execution, all while reducing in-house administrative burdens, operational risks and HR costs. We serve as an extension to your benefits team by offering key resources to allow employers to focus on more strategic initiatives.
We’re here to help
Learn how we can help your business
